News
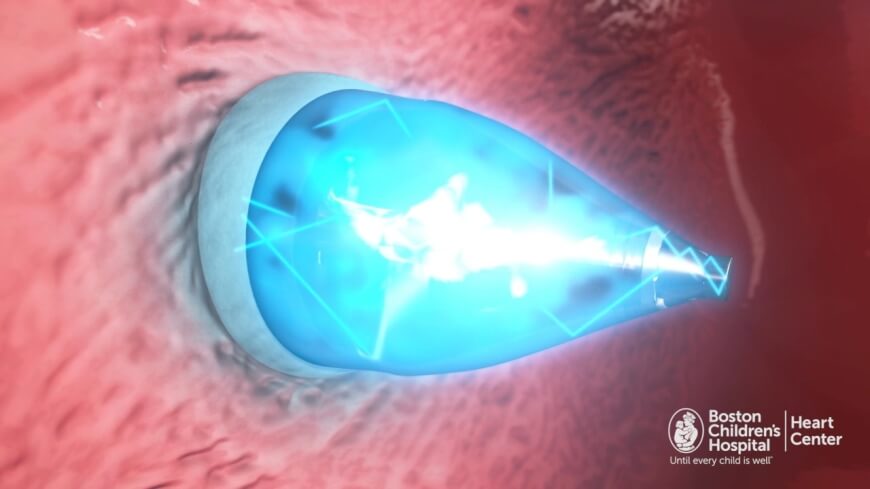
The clinician turns on the catheter’s UV light, which activates the adhesive glue on the patch, connecting it to the heart wall.
Researchers from Boston Children’s Hospital, the Wyss Institute for Biologically Inspired Engineering at Harvard University, Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and the Karp Lab at Brigham and Women’s Hospital have jointly designed a specialized catheter for fixing holes in the heart using a biodegradable adhesive and patch. As the team reports in Science Translational Medicine, the catheter has been used successfully in animal studies to facilitate hole closure without the need for open heart surgery.
Pedro delNido, MD, Chief of Cardiac Surgery at Boston Children's and contributing author on the study, says the device represents a radical change in the way these kinds of cardiac defects are repaired. “In addition to avoiding open heart surgery, this method avoids suturing into the heart tissue, because we’re just gluing something to it.”
Catheterizations are preferable to open heart surgery because they don’t require stopping the heart, putting the patient on bypass, and cutting into the heart. The Heart Center at Boston Children’s is committed to pursuing the least invasive methods possible to correct heart defects, which are among the most common congenital defects.
Last winter, the unique adhesive patch was published in Science Translational Medicine. This represented a large step forward in the quest to reduce complications associated with heart defect repair. While medical devices that remain in the body may be jostled out of place or fail to cover the hole as the body grows, the patch allows for heart tissue to create its own closure and then dissolves.
To truly realize the patch’s potential, however, the Boston Children’s/Wyss/SEAS/Brigham and Women’s research team sought a way to deliver the patch without open heart surgery. Their newly designed catheter device utilizes UV light technology and can be used to place the patch in a beating heart.
The catheter is inserted through a vein in the neck or groin and directed to the defect within the heart. Once the catheter is in place, the clinician opens two positioning balloons: one around the front end of the catheter, passing through the hole, and one on the other side of the heart wall.
The clinician then deploys the patch and turns on the catheter’s UV light. The light reflects off of the balloon’s shiny interior and activates the patch’s adhesive coating. As the glue cures, pressure from the positioning balloons on either side of the patch help secure it in place.
Finally, both balloons are deflated and the catheter is withdrawn. Over time, normal tissue growth resumes and heart tissue grows over the patch. The patch itself dissolves when it is no longer needed.
"This really is a completely new platform for closing wounds or holes anywhere in the body," says Conor Walsh, Ph.D., Wyss Institute Core Faculty member, Assistant Professor of Mechanical and Biomedical Engineering at SEAS, founder of the Harvard Biodesign Lab at SEAS, and author on the paper. "The device is a minimally invasive way to deliver a patch and then activate it using UV light, all within a matter of five minutes and in an atraumatic way that doesn't require a separate incision."
SEAS/Wyss Institute’s Ellen Roche, Ph.D., co-first author on the paper along with Boston Children’s Assunta Fabozzo, M.D., adds that the device is designed to be customizable. For instance, the rate at which the patch biodegrades can be slowed or accelerated depending on how quickly the surrounding tissue grows over it. Further studies will reveal the appropriate lengths of time for different circumstances.
Jeff Karp, Ph.D., a bioengineer at Brigham and Women’s Hospital and a co-founder of Gecko Biomedical, developed the glue product in his lab at Brigham and Women’s Hospital. Gecko Biomedical will be testing the glue product in humans later this year.
“Our collaboration across hospitals and institutions to find new and minimally invasive applications for this glue in clinical settings is a great multi-disciplinary example,” Karp said. “We are translating our discoveries in the lab into solutions for patients.”
“The way the glue works in the face of blood is revolutionary. We don’t have to stop the heart,” says delNido. “This will enable a wide range of cardiac procedures in the future.”
Boston Children’s Hospital is home to the world’s largest research enterprise based at a pediatric medical center, where its discoveries have benefited both children and adults since 1869. More than 1,100 scientists, including seven members of the National Academy of Sciences, 11 members of the Institute of Medicine and 10 members of the Howard Hughes Medical Institute comprise Boston Children’s research community. Founded as a 20-bed hospital for children, Boston Children’s today is a 397-bed comprehensive center for pediatric and adolescent health care. Boston Children’s is also the primary pediatric teaching affiliate of Harvard Medical School. For more, visit our Vector and Thriving blogs and follow us on our social media channels: @BostonChildrens, @BCH_Innovation, Facebook and YouTube.
The Wyss Institute for Biologically Inspired Engineering at Harvard University uses Nature's design principles to develop bioinspired materials and devices that will transform medicine and create a more sustainable world. Wyss researchers are developing innovative new engineering solutions for healthcare, energy, architecture, robotics, and manufacturing that are translated into commercial products and therapies through collaborations with clinical investigators, corporate alliances, and formation of new start–ups. The Wyss Institute creates transformative technological breakthroughs by engaging in high risk research, and crosses disciplinary and institutional barriers, working as an alliance that includes Harvard's Schools of Medicine, Engineering, Arts & Sciences and Design, and in partnership with Beth Israel Deaconess Medical Center, Brigham and Women's Hospital, Boston Children's Hospital, Dana–Farber Cancer Institute, Massachusetts General Hospital, the University of Massachusetts Medical School, Spaulding Rehabilitation Hospital, Boston University, Tufts University, and Charité – Universitätsmedizin Berlin, University of Zurich and Massachusetts Institute of Technology.
The Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) serves as the connector and integrator of Harvard’s teaching and research efforts in engineering, applied sciences, and technology. Through collaboration with researchers from all parts of Harvard, other universities, and corporate and foundational partners, we bring discovery and innovation directly to bear on improving human life and society. For more information, visit http://seas.harvard.edu.
Brigham and Women’s Hospital (BWH) is a 793-bed nonprofit teaching affiliate of Harvard Medical School and a founding member of Partners HealthCare. BWH has more than 4.2 million annual patient visits and nearly 46,000 inpatient stays, and is the largest birthing center in Massachusetts. The Brigham’s medical preeminence dates back to 1832, and today that rich history in clinical care is coupled with its national leadership in patient care, quality improvement and patient safety initiatives, and its dedication to research, innovation, community engagement, and educating and training the next generation of health care professionals. Through investigation and discovery conducted at its Brigham Research Institute (BRI), BWH is an international leader in basic, clinical and translational research on human diseases, more than 1,000 physician-investigators and renowned biomedical scientists and faculty supported by nearly $600 million in funding. To learn more, please visit BWH’s online newsroom.
Cutting-edge science delivered direct to your inbox.
Join the Harvard SEAS mailing list.
Press Contact
Leah Burrows | 617-496-1351 | lburrows@seas.harvard.edu